When you are diagnosed with diabetes, you might initially feel overwhelmed and helpless. This chronic condition isn’t easy to live with all the time, since there are physical side effects of diabetes, as well as emotional and mental effects.
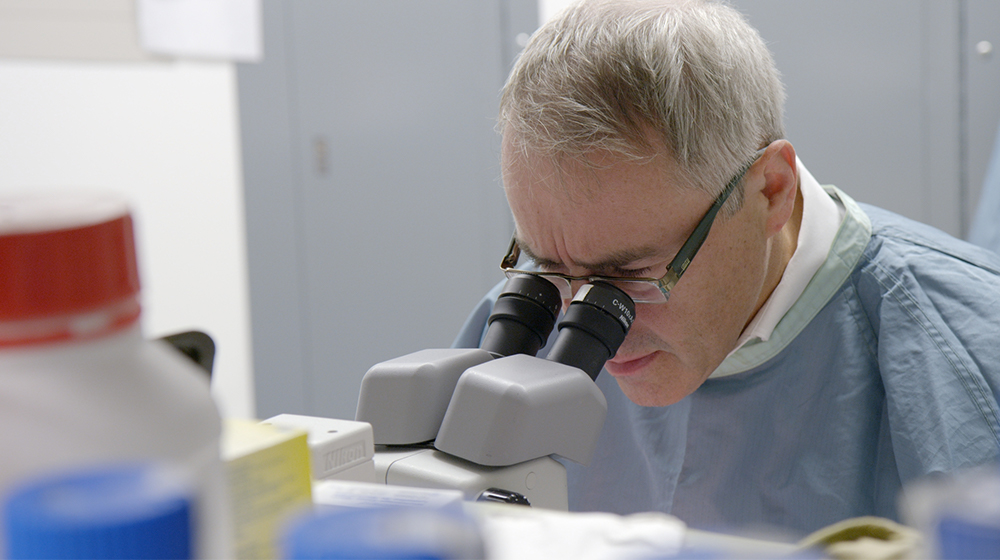
Fortunately, there is active research being done to help uncover a cure, including studies conducted by ProtoKinetix’s principal investigators. While a day in the life of a patient living with diabetes may be a challenging one today, we are working toward a more hopeful tomorrow.
Continue reading to learn how you could be diagnosed with diabetes, learn about current treatments, and discover how ProtoKinetix is helping to research a potential cure.
Getting a Type 1 Diabetes Diagnosis
If your doctor notices that you have symptoms of diabetes, they will administer a few tests. Possible symptoms include increased thirst and hunger, blurred vision, fatigue and unexplained weight loss.
The first test is the random plasma glucose (RPG) test, which measures your blood glucose level. If the RPG test shows a glucose value of 200 milligrams per deciliter, or mg/dL, you have diabetes.
The next blood test – the A1C test – shows how long you’ve had high blood glucose. The A1C test shows your average blood glucose levels as a percentage over the previous three months. If you are between 5.7% and 6.4%, you are most likely pre-diabetic. A result of 6.5% or higher shows you have diabetes.
These tests will determine whether or not you have diabetes. However, if you do, they will not tell you if it’s Type 1 or Type 2. That’s where testing the blood for autoantibodies comes into play. Certain autoantibodies will accidentally attack healthy cells and tissues. This occurs in Type 1 diabetes, where the pancreas has been damaged and can no longer make insulin.
Daily Challenges of Living with Type 1 Diabetes
Currently, there is no cure for diabetes, so living with the chronic condition has its ups and downs. Diabetes takes a toll on both your physical and mental health, so it is important to take steps to support your emotional wellness as you go through the journey of managing the disease.
If you have diabetes, you will find yourself checking your blood sugar multiple times a day in order to adjust the amount of insulin you’re taking. Most people assume the sugar you eat is the only thing you need to track. In reality, all carbohydrates need monitored. And, since exercise affects blood sugar levels, that needs to be considered as well.
This constant monitoring and planning can be exhausting, especially when combined with feelings of fatigue caused by lack of sleep or high blood sugar (both symptoms of diabetes).
Managing a chronic condition can also cause emotional distress. This can lead to mood swings and feelings of depression.
The people around you – family, friends, co-workers and even strangers – might think they know what’s best for you. For example, they might nag you about taking insulin or comment on your food choices. But you and your health care provider will know what’s best for you.
The thing to remember is this: You are not your illness. You learn how it affects you and work with that information.
Side Effects of Type 1 Diabetes
Diabetes can affect many parts of your body. Let’s start from the top.
Compared with those who don’t have diabetes, you’ll have an increased risk of glaucoma and cataracts. The blood vessels in the eyes can become damaged, causing visual disturbances and eventually blindness if left untreated. Blood vessels throughout the body become damaged by having too much glucose in your blood.
If you have diabetes, you’re also at a higher risk for heart disease due to the increased risks of high blood pressure from damaged blood vessels. With diabetes-related kidney and pancreas problems, fatigue and a lack of concentration can set in.
High blood sugar can result in dry, cracked skin. The additional sugar causes your body to lose fluids more quickly. The body tries to remove this overload by frequent urination. On the other hand, moist, warm areas of the skin – such as between the fingers and toes, armpits and the groin – are easy targets for fungal, bacterial or yeast infections, who thrive on glucose.
Feeling tingly sensations in your legs? Diabetes can cause nerve damage, which can lead to a “pins and needles” sensation as well as the inability to sense pain or changes in temperature. This increases the risk of injuries, and those injuries may have a difficult time healing and lead to infection.
And now, down to the feet. This is the area in which people usually relate diabetic injuries. Because of poor blood flow and nerve damage, those with diabetes have an increased risk of infections, ulcers and calluses. This can lead to amputations of the foot and leg.
The physical effects of Type 1 diabetes can be severe. However, treatments are available.
Looking for Hope: Type 1 Diabetes Treatment Options
In order to keep your blood sugar at a normal level, you’ll need to take insulin. There are different types, including short-acting insulin, rapid-acting insulin, intermediate-acting (NPH) insulin and long-acting insulin.
There are two ways of getting insulin into the body: injections and an insulin pump. Injections can be administered with a fine needle and syringe or an insulin pen multiple times a day. One type of insulin pump is worn on the abdomen to connect its insulin reservoir to a catheter inserted under the skin. The other type is wireless. An insulin pump offers a steady dose of insulin throughout the day. You’ll need to program it when you eat to offset a spike in blood sugar. Sometimes the combination of a sensor with a pump is called an artificial pancreas.
Medications such as high blood pressure medication and cholesterol-lowering drugs can be prescribed if you have related symptoms. Taking aspirin daily might be advised as well for heart health. Seeing your doctor regularly is your best opportunity to maximize your health.
Medical procedures that are being studied as treatments for Type 1 diabetes include pancreas transplants and islet cell transplantation. Pancreas transplants would ensure that you would no longer need to take insulin; however, they’re not always successful. This risky procedure is for those who also need a kidney transplant or have a hard time managing their diabetes.
Islet cell transplantation involves the use of islet cells from a donor that are transplanted into a patient with Type 1 diabetes. These cells will then help produce insulin. However, this procedure isn’t always effective. Because of this, researchers like Dr. James Shapiro are studying ways to improve islet cell transplants with the anti-aging glycopeptide, AAGP®.
The Potential Benefits of AAGP®
Islet cell transplantation doesn’t always work because the body will try to reject the donor’s cells. ProtoKinetix is leading the way on studying AAGP® used in tandem with islet cells.
The Shapiro Group, led by Dr. Shapiro, has been working with the most unstable diabetes patients to determine the viability for AAGP® to keep cells alive and allow for successful islet cell transplants. In these studies, islet cells are taken from donors and transplanted into patients with Type 1 diabetes using AAGP® to help stabilize them.
ProtoKinetix is also in the discovery phase of AAGP®’s effects on whole organ support. This can help those who undergo retinal grafts to help with diabetic retinopathy. AAGP® can help keep retina cells viable. Future work done by ProtoKinetix will expand to develop AAGP® in concert with ongoing developments that support whole organs, such as the pancreas, heart and liver, for transplantation.
The future can be very hopeful for those living with diabetes.
Explore investment opportunities
The research exploring the potential for AAGP® as a diabetes treatment option has been extremely promising thus far, but to continue our investigations, we need the support of dedicated investors. If you are interested in investing in the potential, please talk to your broker or contact the team at ProtoKinetix to explore potential investment opportunities. This is an incredible opportunity to be involved in the next great medical discovery, and we hope you’ll join us.